Reverting five years of progress: Impact of COVID-19 on maternal mortality in Peru
Maternal health not considered core in COVID response
Increased risk of maternal deaths
Restrictions on preventive and emergency services
COVID not the main cause of increase in maternal deaths
How to cite this publication:
Camila Gianella, Jorge Ruiz-Cabrejos, Pamela Villacorta, Andrea Castro, Gabriel Carrasco-Escobar (2021). Reverting five years of progress: Impact of COVID-19 on maternal mortality in Peru. Bergen: Chr. Michelsen Institute (CMI Brief 2021:1)
Spanish version: Revertir cinco años de progreso: El impacto de la covid-19 en la mortalidad materna en Perú
Peru has moved back at least five years on its road to reducing maternal mortality, due to the profound impact COVID-19 has had on the capacity of health services. Our research shows that the health system needs urgent reengineering. Among other things, we recommend including pregnant woman in the COVID-19 risk groups.
Since the early 1990s, Peru has seen a major decline in the maternal mortality ratio. In fact, the country was well on its way to achieving Sustainable Development Goal 3 (SDG3) target 3.1, which aims to reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 2030. But the COVID-19 pandemic has led to dramatic setbacks. Peru swiftly implemented strict measures to control the spread of the virus, such as closing borders, restricting freedom of movement nationwide, banning crowds, and closing schools, universities, and churches. It also restricted all non-essential activities or services, including non-emergency primary health services. Despite these actions, it is among the countries with the highest COVID-19 incidence and mortality rates in Latin America and the Caribbean, as well as globally (Johns Hopkins University Coronavirus Resource Center 2020, The Economist 2020). This Brief aims to show the impact that the COVID-19 pandemic has had on the maternal mortality trajectory in Peru.
Maternal health not considered core in COVID response
This analysis contributes to the COVID-19 debate by analysing the pandemic’s direct and indirect impact on maternal mortality in Peru. There are a number of reasons why we focus on maternal mortality. First, in an emergency context where health systems have been put under pressure, it is important to understand what has been prioritised, as well as the different ways in which shutting down essential health services affect different population groups disproportionally. There is an emerging body of literature describing the impact on emergency services, including antenatal and neonatal services (Garrafa, Levaggi et al. 2020, Reinders, Alva et al. 2020). The effect that this has had on health outcomes needs to be understood more thoroughly. Second, the literature describes how maternal mortality indicators are sensitive to the health system’s capacity to provide quality health services, at the primary level, as well as its capacity to refer to complex care. What is more, maternal mortality is sensitive to social inequity and socioeconomic marginalisation.
Maternal mortality focuses on a group in the population, women, of reproductive age, that in the context of the pandemic has not been identified as a high-risk group by most health authorities, in Peru or worldwide. At the beginning of the pandemic, the main concern around pregnant women was to prevent the exposure of the foetus to the disease. Health agencies did not consider maternal health or mortality risk to be a core issue. Early evidence showed a lower risk for women (grouping all of them and neglecting particular vulnerable groups). Meanwhile, the data collected, mainly from China, and Europe, did not indicate that pregnant women were at higher risk to develop severe symptoms due to SARS-CoV-2. There were almost no reported maternal deaths (Takemoto et al. 2020). Importantly, researchers excluded pregnant women from COVID-19 treatment trials, even when the treatment being evaluated had no or low safety concerns during pregnancy (Taylor, Kobeissi et al. 2020).
Increased risk of maternal deaths
By the end of 2020, evidence was showing that pregnant women were potentially more likely to need intensive care treatment for COVID-19 (Allotey et al. 2020). In addition, conditions related to high-risk pregnancies (such as pre-existing comorbidities, high maternal age, and high body mass index) now seemed to be risk factors for severe COVID-19 (Allotey, Stallings et al. 2020, Zambrano, Ellington et al. 2020). Evidence from low- and middle-income countries that are highly affected by the pandemic, like Iran or Brazil, indicates that there is a possibility of increased risk of maternal deaths due to COVID-19 (Takemoto, Menezes et al. 2020). However, there is still limited information on the effect of the pandemic response on maternal services and maternal health. This is within a context where across the globe, many countries, including middle- and low-income countries, are facing second waves of COVID-19 outbreaks. Therefore, it is important that studies generate evidence to correct COVID-19 responses and protect vulnerable groups of the population.
As with other health conditions, including COVID-19, maternal mortality is unevenly distributed across Peru. Reports from 2019 show that the Amazon regions of Ucayali, Amazonas, Madre de Dios, and Loreto reported maternal mortality ratios (MMR) that are far above the national indicators (Gil 2018).
The main causes of maternal deaths in Peru are haemorrhage, hypertension (related to eclampsia and pre-eclampsia), and abortion complications. In the case of pregnancy-related death, the causes are suicide, cancer, and respiratory tract infections (Gil 2018, Centro Nacional de Epidemiología Prevención y Control de Enfermedades 2020). In Peru, three out of five maternal deaths occur in the puerperium period (42 days after delivery) (UNFPA 2020).
Restrictions on preventive and emergency services
Formally, all pregnant women residing in the country have the right to access to antenatal and postnatal health care. In April 2020, Peru’s Ministry of Health (MoH), issued an order to guarantee access to antenatal, perinatal, and postpartum care during the COVID-19 emergency. Yet preventive services, as part of primary health care, were suspended for around two and a half months(Mesa de Consertación de Lucha Contra la Pobreza 2020). Despite the MoH plans, across the country obstetric outpatient services also remained restricted up until the end of 2020(Reinders, Alva et al. 2020, UNFPA 2020). Within the context of COVID-19 second wave, it is still uncertain when the services will be reopened. At the same time, access to emergency health care was also limited for many months due to the absence of health personnel. It has been reported that intensive care units for pregnant women have been reallocated to COVID-19 patients (UNFPA 2020).
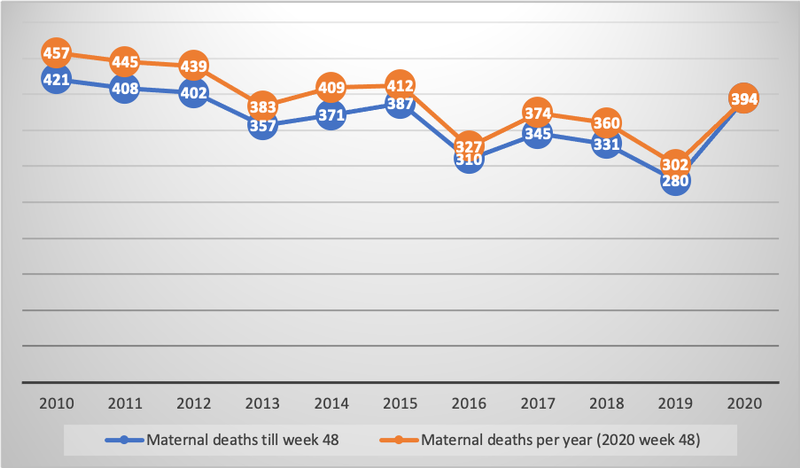
The Ministry of Health has reported an increase in maternal deaths (see Figure 1). However, it is not yet clear how many of these were directly linked to COVID-19 infection and/or as a consequence of lack of timely access to health care.
Study method and findings
We used the data from the national death registry information system (SINADEF is the Spanish acronym) from 2017 to the 28 November 2020. SINADEF contains individual data on gender, age, district of residence, civil status, insurance, and education at the moment of death, along with the causes of death (direct, underlying, or associated) in ICD-10 codes (World Health Organization 2019). However, 22.72% of registered deaths did not have any cause of death reported. For our analysis, the inclusion criteria for a record to be classified as a ‘maternal death’ was any woman, between the age of 12 and 57 (the oldest reported maternal age by the MoH)(Ministerio de Salud and Centro Nacional de Epidemiología Prevención y Control de Enfermedades 2020), that had at least one cause of death labelled as ‘pregnancy, childbirth and postnatal’, which includes all ICD-10 codes in the range O00–O99. Additionally, a registered death was categorised as a ‘COVID-19 related death’ if at least one of the six causes of death was coded under chapter U07 (ICD-10 code for SARS-CoV-2). After including those that fulfilled these criteria, we selected a total of 442 registered deaths for further analysis.
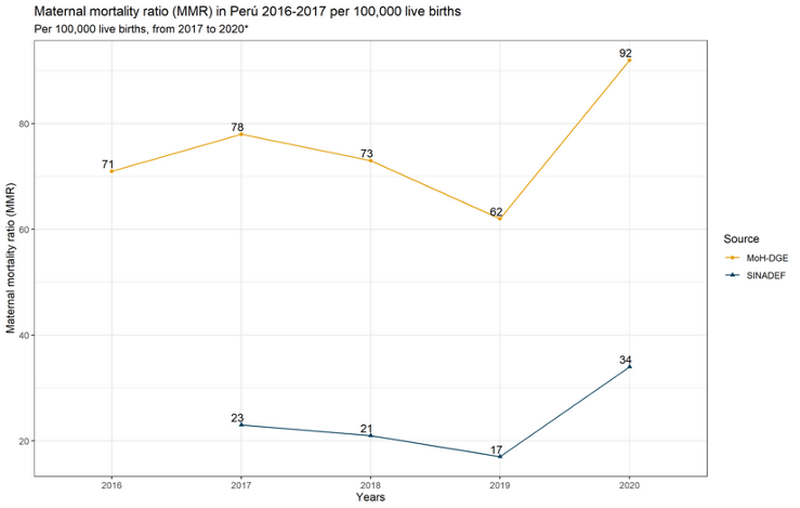
Our analysis shows an increase in maternal deaths, from 83 deaths in 2019, up to 146 during 2020 (to November). This is a 75% increase. When adjusted for live births, the increase in maternal mortality ratio (MMR) goes from 17 maternal deaths per 100,000 live births in 2019 to 34 maternal deaths per 100,000 live births. This shows a 102% increase in the data collected by SINADEF. The MMR increased from 62 to 92 when calculated from the MoH totals (Figure 2). This increase represents a major disruption given that maternal mortality in the country had previously reduced two years in a row (Figure 1).
COVID not the main cause of increase in maternal deaths
Out of the 146 maternal deaths reported in the period included in this analysis, 35 (23.97%) were categorised as COVID-19 cases. The mean age for both groups at the moment of death was similar, with a mean of 31 for COVID-19 cases and a mean of 30 for those for whom COVID-19 was not recorded. The age ranges went form 15 – 45 for COVID cases and 16 – 48 for non COVID cases.
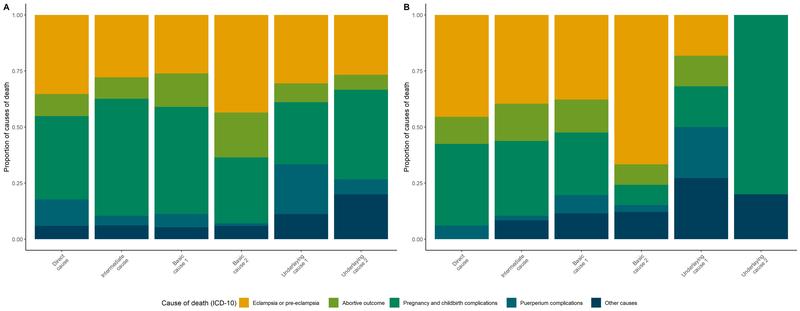
The data on cause of death indicate that COVID-19 infection was not the main reason behind the increase in maternal deaths. Without the COVID-19 cases, there was an increase of 33% in the number of maternal deaths between 2019 and 2020. Our analysis of causes of death shows that women lacked timely health care. Figure 3 (graph A corresponds to the years 2017–19 while graph B corresponds to 2020), shows an increase on the proportion of cases where preeclampsia/eclampsia appeared as the main, or principal, underlying cause of deaths in 2020. It should be noted that the principal risk factors for death in women with preeclampsia/eclampsia are a lack of prenatal care, associated with chronic hypertension (Amorim, Santos et al. 2001). Lack of antenatal care does not allow timely diagnosis of high-risk pregnancies due to for example preeclampsia. The rise in childbirth complications (including preterm delivery, intrauterine growth restriction, abnormal placenta, detection of congenital malformations, and haemorrhage, among others) also indicates lack of antenatal control for timely diagnosis of some conditions, as well as a lack of access to emergency obstetric care. During the COVID-19 pandemic, health services have been saturated and intensive care units for pregnant women have decreased (UNFPA 2020).
Conclusion and policy recommendations
COVID-19, as a health condition, contributes to maternal mortality. Peru has moved back at least five years on its path to reducing maternal mortality (see Figure 1). Although pre-pandemic trajectories could be recovered once extensive vaccinations have been undertaken, this Brief highlights the weakness of a health system that needs urgent re-engineering to guarantee access to health services to those that require care.
Recommendations
Following on from this study, the authors make the following recommendations:
- The need to re-examine COVID-19 risk groups to include pregnant women, and to call governments to develop and implement measures to protect this group of the population from COVID-19 infections. This is especially given that there are valid safety concerns to include pregnant women as priority group for COVID-19 vaccines.
- That truly comprehensive approaches to pregnant women should be developed. Diseases, such as malaria, have already show the risks that pregnancy creates for women. The health of pregnant women should receive the same level of interest as vertical transmission from the medical community.
- In the context of calls for new lockdown measures as a means to control second waves of COVID-19, there is a need to guarantee the provision of essential services such as antenatal care.
- It is also important that open data sources inform decisions. SINADEF is a positive example; however, the superposition of different records of death limits the capacity to perform comprehensive analyses. National registers such as SINADEF must include all deaths, including maternal deaths. Some of the weakness of this analysis – for example, the differences between the gross data reported on maternal deaths by the MoH and the data from SINADEF – are rooted in the lack of clarity or omission in the initial reports, and the presence of different overlapping systems. Accurate information on maternal deaths is registered as part of the Surveillance System of the National Center for Epidemiology and Disease Control (CDC-Peru). This information is not open access and is under control of Peru’s Ministry of Health (the team in charge of this study formally asked for access to the information, but the request was not answered). However, as mentioned above, when compared annually, both sources follow a consistent trend.
- It is important to assess the impact of COVID-19 pandemic, beyond the number of COVID related deaths. The devastating effects of COVID-19 on health systems are contributing to excess mortality. It is important to understand how this is distributed among the population, which groups are more vulnerable.
References
Allotey, J., E. Stallings, M. Bonet, M. Yap, S. Chatterjee, T. Kew, L. Debenham, A. C. Llavall, A. Dixit, D. Zhou, R. Balaji, S. I. Lee, X. Qiu, M. Yuan, D. Coomar, M. van Wely, E. van Leeuwen, E. Kostova, H. Kunst, A. Khalil, S. Tiberi, V. Brizuela, N. Broutet, E. Kara, C. R. Kim, A. Thorson, O. T. Oladapo, L. Mofenson, J. Zamora and S. Thangaratinam (2020). ”Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis.” BMJ 370: m3320.
Amorim, M. M. R. d., L. C. Santos, A. M. F. Porto and L. K. D. Martins (2001). ”Risk factors for maternal death in patients with severe preeclampsia and eclampsia.” Revista Brasileira de Saúde Materno Infantil 1: 237-247.
Centro Nacional de Epidemiología Prevención y Control de Enfermedades (2020). Muerte Materna. http://www.dge.gob.pe/portal/docs/tools/teleconferencia/2020/SE412020/04.pdf, Ministerio de Salud.
Garrafa, E., R. Levaggi, R. Miniaci and C. Paolillo (2020). ”When fear backfires: Emergency department accesses during the Covid-19 pandemic.” Health Policy 124(12): 1333-1339.
Gil, F. (2018). Situación Epidemiológica de la muerte materna en el Perú.
Johns Hopkins University Coronavirus Resource Center. (2020). ”COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins”. Retrieved October 6, 2020, from https://coronavirus.jhu.edu/map.html.
Mesa de Consertación de Lucha Contra la Pobreza (2020). Informe nacional sobre el impacto del COVID-19 en las dimensiones económica, social y en salud en el Perú (al mes de mayo, 2020). Incluye hallazgos de 16 mesas regionales. https://www.mesadeconcertacion.org.pe/storage/documentos/2020-08-17/informe-salud-mclcp-2020-7-de-julio.pdf, Mesa de Consertación de Lucha Contra la Pobreza.
Ministerio de Salud and Centro Nacional de Epidemiología Prevención y Control de Enfermedades (2020). Número de muertes maternas anual y hasta la SE 48, 2000 - 2020. https://www.dge.gob.pe/portal/docs/vigilancia/sala/2020/SE48/mmaterna.pdf, Ministerio de Salud.
Reinders, S., A. Alva, L. Huicho and M. M. Blas (2020). ”Indigenous communities’ responses to the COVID-19 pandemic and consequences for maternal and neonatal health in remote Peruvian Amazon: a qualitative study based on routine programme supervision.” BMJ Open 10(12): e044197.
Takemoto, M. L. S., M. O. Menezes, C. B. Andreucci, R. Knobel, L. A. R. Sousa, L. Katz, E. B. Fonseca, C. G. Magalhães, W. K. Oliveira, J. Rezende-Filho, A. S. O. Melo and M. M. R. Amorim (2020). ”Maternal mortality and COVID-19.” The Journal of Maternal-Fetal & Neonatal Medicine: 1-7.
Taylor, M. M., L. Kobeissi, C. Kim, A. Amin, A. E. Thorson, N. B. Bellare, V. Brizuela, M. Bonet, E. Kara, S. S. Thwin, H. Kuganantham, M. Ali, O. T. Oladapo and N. Broutet (2020). ”Inclusion of pregnant women in COVID-19 treatment trials: a review and global call to action.” The Lancet Global Health.
The Economist (2020) ”Tracking covid-19 excess deaths across countries. In many parts of the world, official death tolls undercount the total number of fatalities.”
UNFPA (2020). Muertes maternas aumentarán en 40% debido a la pandemia si no se recupera el sistema de salud. UNFPA https://peru.unfpa.org/es/news/muertes-maternas-aumentar%C3%A1n-en-40-debido-la-pandemia-si-no-se-recupera-el-sistema-de-salud.
Zambrano, L. D., S. Ellington, P. Strid, R. R. Galang, T. Oduyebo, V. T. Tong, k. R. Woodworth, J. F. Nahabedian, E. Azziz-Baumgartner, S. M. Gilboa and D. Meaney-Delman (2020). ”Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–October 3, 2020.” MMWR Morb Mortal Wkly Rep (69): 1641–1647.



