Direct health facility financing in Tanzania. Process evaluation. Phone Survey #3
Training and knowledge about RBF indicators
Difficult RBF indicators to improve
Direct Health Facility Financing (DHFF)
Training and knowledge of DHFF indicators
Understanding patterns in service delivery
Results: Community health worker survey
RBF training and knowledge of RBF indicators
RBF and community health worker performance
Community health worker performance
Challenges in improving performance
Understanding patterns in service delivery
Observed changes in HW behaviour
Perceptions of stunting prevalence
How to cite this publication:
Peter Binyaruka, Ottar Mæstad, Vincent Somville (2021). Direct health facility financing in Tanzania. Process evaluation. Phone Survey #3. Bergen: Chr. Michelsen Institute (CMI Report 2021:09)
CMI Brief 2021:5: Towards harmonised financing of frontline health service providers in Tanzania.
CMI Report 2021:07: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #1.
CMI Report 2021:08: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #2.
CMI Report 2021:10: Direct Financing of Health Facilities. Experiences from financing reforms in Tanzania.
Introduction
Background
The Government of Tanzania is currently implementing a Results-Based Financing (RBF) scheme in nine regions. The scheme is designed to improve health service use and equity, as well as the quality and efficiency of health care, particularly among primary health care facilities.
Since 2015, the Ifakara Health Institute (IHI), in collaboration with the London School of Hygiene and Tropical Medicine (LSHTM) and Chr. Michelsen Institute (CMI), has conducted a rigorous impact and process evaluation of the RBF scale-up, focusing on the Mwanza region.
As part of the process evaluation, the research team has previously conducted two rounds of phone-interviews with all health workers (HWs) and community health workers (CHWs) who participated in the baseline survey in the Mwanza region in 2016. The first round was conducted in February 2018 and the second in November the same year.
From 2017/2018, the Government of Tanzania has also implemented Direct Health Facility Financing (DHFF) in all regions. The DHFF reform involves the transfer of health basket funds directly from the Ministry of Finance and Planning to health facility bank accounts and has similar objectives to the RBF programme.
This brief report summarizes the findings from a third phone survey, conducted in November 2020. The survey had two main objectives:
- To shed light on findings from the RBF impact evaluation, which conducted its endline survey earlier in 2020.
- To shed light on findings from the RBF-DHFF study, which was conducted in parallel with the RBF endline and assessed which factors facilitated or inhibited the success of the RBF and DHFF programmes.
Topics
This survey covers a variety of topics related to:
- Training in and knowledge of the RBF and DHFF programmes.
- RBF and DHFF implementation, including the impact of delayed payments.
- Impacts of RBF and DHFF on service delivery, including their relative importance.
- Understanding patterns in service delivery.
Data collection and sample
Participants in the phone survey are health workers (HWs) and community health workers (CHWs) who participated in the endline survey of the RBF impact evaluation. Unlike previous phone surveys, which focused on the Mwanza region only, this survey also included participants from the Mara region. Mara has been the control region for the impact evaluation, as RBF was not implemented in Mara until late 2019.
We aimed to interview two HWs and two CHWs at each of the 150 facilities in the sample (75 facilities in each region), a total of 300 HWs and 300 CHWs. The health facilities were randomly selected at baseline and so were the participating HWs and CHWs.
A total of 591 respondents were interviewed: 297 CHWs (149 in Mwanza and 148 in Mara) and 294 HWs (148 in Mwanza and 146 in Mara). The phone survey was conducted in mid-November 2020 by a professional survey company, Economic Development Initiatives (EDI), based in Bukoba-Kagera.
Results: Health worker survey
The health workers interviews focused on the following topics:
- Results-based Financing
- RBF training and knowledge of RBF indicators
- RBF indicators that are difficult to improve
- RBF payments
- RBF design
- Direct Health Facility Financing
- DHFF training and knowledge of DHFF performance indicators
- DHFF implementation (including infrastructure)
- RBF and DHFF compared
- Understanding patterns in service delivery
- Institutional deliveries
- Use of contraceptives
- Growth monitoring of children
Results-based Financing
Training and knowledge about RBF indicators
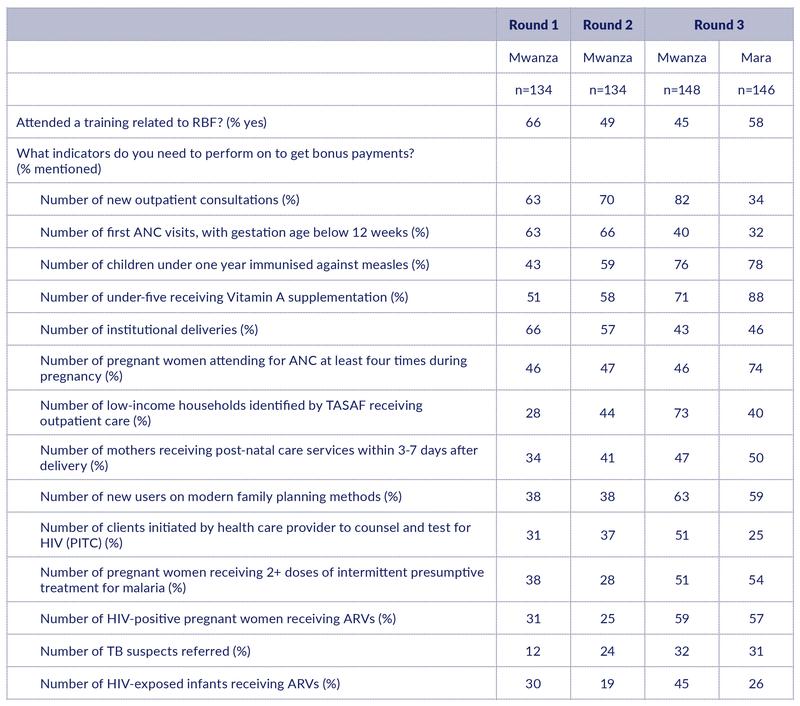
There is a declining trend in the share of health workers reporting to have attended RBF training (Table 1). In Mwanza, 66% of the interviewed health workers had attended RBF training in February 2018. The share is down to 45% in this round. The share is higher in Mara (58%), though, probably because RBF training in Mara was conducted more recently, in mid-2019.
As a measure of HW knowledge about RBF indicators, we asked HWs to mention those services that count in the calculation of RBF bonus payments (open question). Out of 14 incentivised services, HWs were able to mention 7.8 services in Mwanza. This is a significant improvement from Round 2, when they were able to mention 6 services. This suggests that knowledge about the RBF programme is maintained and strengthened over time, despite a reduction in the share of health workers who have attended formal training. In Mara, HWs were able to mention 6.9 services on average.
While there are improvements on most indicators, there are a couple of observations that point in the opposite direction. There is a significant reduction in the share of HWs who mention institutional deliveries and early ANC as RBF indicators. Only around 40% of the HWs mention these indicators in this round, compared to around 60% in previous rounds.
The services that are most commonly recalled are vitamin A supplements and measles vaccination for children (mentioned by around 80%). The service that is recalled by the fewest HWs is referrals of TB suspects.
Table 1: Training and knowledge about RBF indicators
Difficult RBF indicators to improve
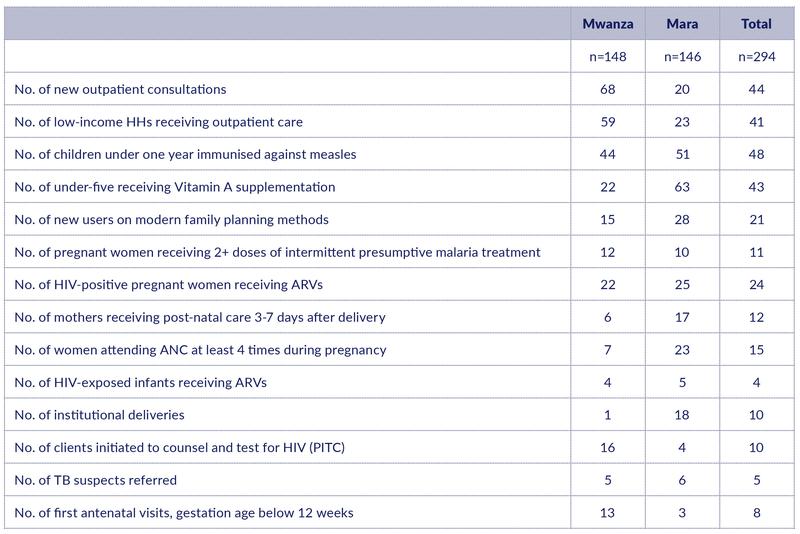
RBF may induce HWs to focus their attention on some services at the expense of others. To improve our understanding of how HWs make such trade-offs, we asked which RBF indicators are most difficult to improve. Each HW was asked to mention the three most difficult indicators to improve.
Table 2 shows which indicators were mentioned as most difficult to improve. In interpreting these figures, we need to keep in mind that HWs are consciously aware of only a sub-set of the RBF indicators. Indicators that they are not conscious of will therefore not be mentioned here, even though they may also be difficult to improve.
In Mwanza, the top three indicators that are seen as difficult to improve are new outpatient consultation (mentioned by 68%), low-income households receiving outpatient care (59%), and measles immunisation (44%). In Mara, the two indicators that stand out as most difficult to improve are vitamin A supplementation (mentioned by 63%) and measles immunisation (51%). Note however, that if we instead look at how many mention an indicator as a difficult relative to how many are aware of the indicator, outpatient consultations stand out as a difficult indicator to improve in Mara as well. The pattern across regions may therefore be more similar than it appears at first glance.
There may be different reasons why indicators are perceived as difficult to improve; some indicators may be inherently difficult to affect through supply-side measures, because demand-side factors are more important for utilisation; other indicators may be difficult to improve because coverage is high at the outset and a further increase would take substantial resources.
It is also interesting to note which indicators are not mentioned as difficult to improve. For instance, very few health workers in Mwanza included frequent ANC visits, institutional deliveries, or post-natal care within 3-7 days among the difficult ones.
Table 2: Results-Based Financing (RBF) indicators perceived as most difficult to improve (% mentioning the indicator as one of the three most difficult ones).
RBF payments
Delays in RBF payments have been a challenge for RBF implementation. No HWs in Mara had received any RBF payments at the time when this study was conducted – one year and four months after the programme started.
In Mwanza, 85% of the health workers that we interviewed in November 2020 had received RBF payments. Note that some health workers may have been recruited recently and therefore had not received any payments yet.
There was huge variation in the reported timing of the last payment in Mwanza. While only 20% had received any RBF payments in 2020, 56% claimed that their last RBF payment was in 2019, and 24% that it was received in 2018. This variation may however be due to recall bias, as we were informed in the field that a region-wide payment took place around February 2020.
The reported amounts received at the last payment also varied considerably, from less than TSH 100,000 up to several millions. The median amount was TSH 250,000, while the average was close to TSH 700,000. Note that due to the payment delays, some payments may have covered several quarters. This might be one reason for the large variation.
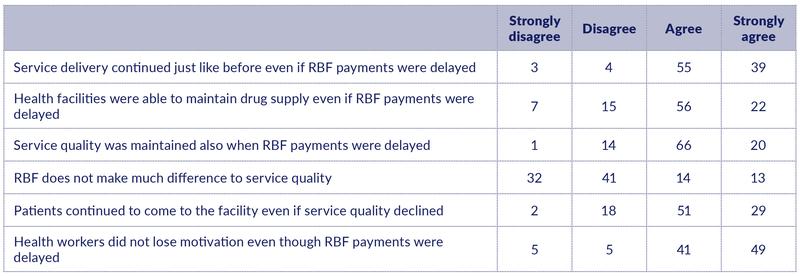
We asked how the delays in RBF payments in Mwanza from 2018 onwards have affected service delivery (Table 3). While HWs claim that RBF contributes significantly to improved services quality, a large majority agree or strongly agree that the delays in payments did not reduce HW motivation (90%) and that service delivery continued just like normal (93%). A high share of health workers also claimed that they were able to maintain drugs supply (78%) and that service quality was maintained (86%). These responses suggest that positive effects of RBF on service provision can be maintained through long periods of delayed RBF payments.
Table 3: Perceived effects of delays in RBF payments in Mwanza from 2018 onwards (%), n=148.
RBF design
RBF payments are split in two parts: 75% is for the facility and 25% is for staff bonuses. One interesting question is what role the staff bonus is playing in improving service quality. We therefore asked health workers how service quality would be affected if all payments instead went to the health facility and nothing went to the HWs.
Figure 1: Perceived effect of letting all RBF payments go to the health facility (%).
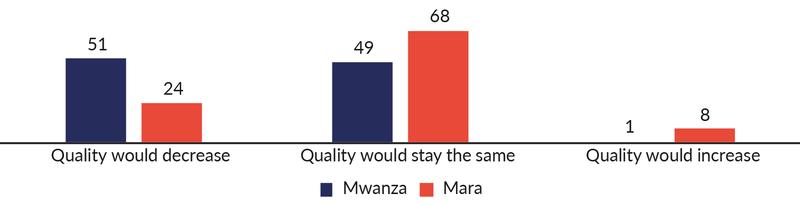
It is noteworthy that even if HWs have an incentive to report that quality would decrease, more than half of them say that quality would stay the same even without a staff bonus.
The responses differ somewhat between Mwanza and Mara; HWs that already have received RBF payments (in Mwanza) think it is more likely that quality will be reduced than those who have not yet received any payments. This suggests that removing the staff bonus is more likely to have a negative effect than simply not implementing a staff bonus in the first place.
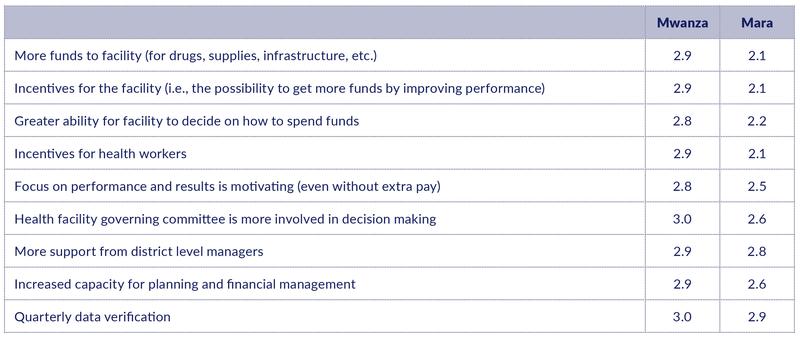
We also asked HWs to rate the importance of various elements of the RBF programme for improving service delivery (Table 4). The various elements were rated as not important (1), somewhat important (2), or very important (3). In Mwanza, almost all HWs rate all elements as very important. Responses in Mara are more nuanced. Interestingly, the elements with the highest score are the ‘softer’ elements of RBF, like increased support from district level and increased capacity for planning and financial management, and not resources and incentives. However, this may reflect the fact that no payments have yet been received. Note also that the element with the highest score in both regions is the quarterly data verification.
Table 4: Importance of elements of Results Based Financing (RBF) for improving service delivery. Average scores. 1 = Not important, 2= Somewhat important, 3 = Very important.
Direct Health Facility Financing (DHFF)
Training and knowledge of DHFF indicators
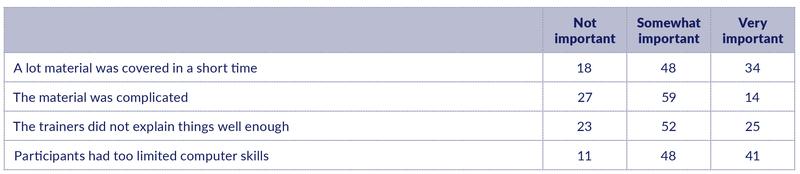
In the RBF-DHFF study, one third of the in-charges reported inadequate training in DHFF. We therefore wanted to know what could explain limited satisfaction with the training.
Surprisingly, only 44 of the health workers interviewed reported that they had participated in DHFF training. Their explanations for limited satisfaction with DHFF training are summarised in Table 5. All the mentioned causes are reported to be somewhat or very important, with limited computer skills among participants and the amount of material covered standing out as the most important explanations.
Table 5: Reasons for limited satisfaction with DHFF training (%), n=44.
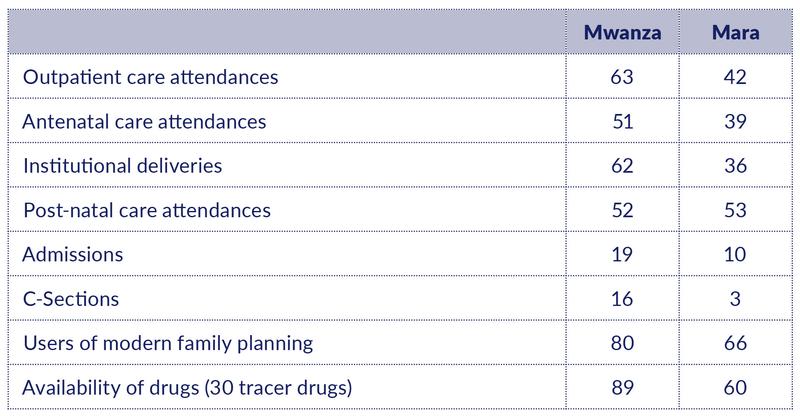
DHFF is allocated to health facilities as the combination of a base tranche (based in indicators such as catchment population and distance to district headquarters) and a performance tranche. The set of performance indicators has expanded over time. We asked HWs to mention which performance indicators they are aware of (Table 6).
The DHFF performance indicators seem to be better known in Mwanza than in Mara. In Mwanza, HWs on average mentioned 4.3 of the 8 performance indicators, while 3.1 indicators were mentioned in Mara. The best-known indicators in both regions are availability of drugs and users of modern family planning.
There is considerable overlap between RBF and DHFF performance indicators. It is noteworthy that in Mwanza, where RBF has been implemented much longer than DHFF, some of the indicators that are part of both programmes (e.g., institutional deliveries, post-natal care, antenatal care, and users of modern family planning) are mentioned by more HWs in connection with DHFF than in connection with RBF (cf. Table 1).
Table 6: DHFF performance indicators mentioned by HWs (%).
DHFF implementation
New digital tools for planning, budgeting, and accounting were implemented along with DHFF. PlanRep is the new planning tool, and in the RBF-DHFF study we noted that a significant share of the in-charges reported that PlanRep was not used to a high extent in planning and budgeting. We wanted to know why. The responses are reported in Table 7.
Table 7: Importance of various constraints for the use of PlanRep (%).
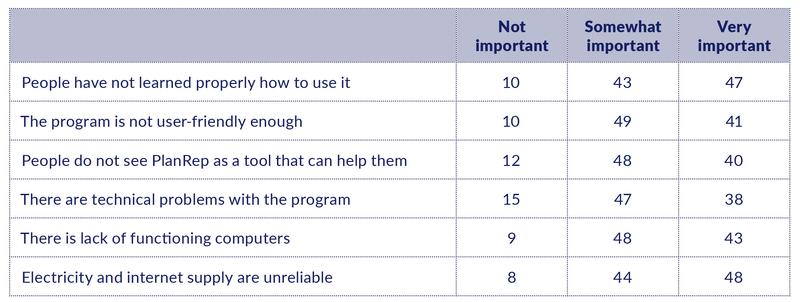
The responses suggest that there is a broad set of factors that contribute to less-than-optimal utilisation of PlanRep. None of the mentioned constraints stand out as significantly more important than the others.
The implementation of the DHFF programme was associated with the introduction of facility accountants to support on financial matters. In Round 2, 89% of health workers in Mwanza acknowledged that their facility had received technical support from an accountant. The figure in Round 3 was down to 82%, while in Mara 88% confirmed to have received such support. The support from accountants was perceived as very important to most health workers (100% in Mwanza and 87% in Mara).
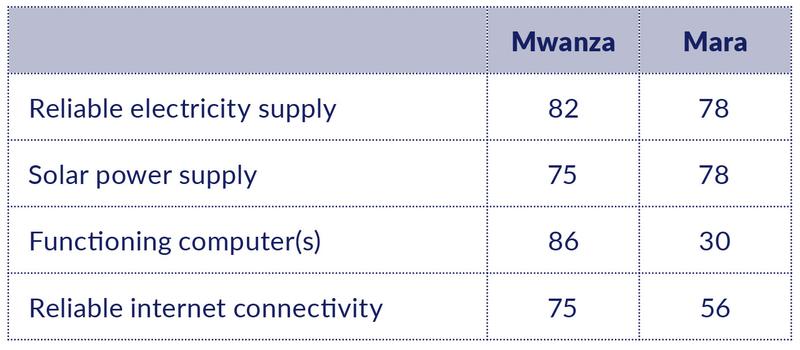
This phone survey also assessed the availability of equipment and utilities that are crucial for well-functioning digital support systems (Table 8). Around 80% of health facilities in the two regions have reliable electricity supply, including solar power. The availability of functioning computer(s) and reliable internet connectivity are also at this level in Mwanza region, but available to far fewer health facilities in the Mara region.
Table 8: Availability of facility equipment and utilities (%).
RBF and DHFF compared
As RBF and DHFF have similar objectives, we were interested in HWs perceptions of which programme has the greatest potential to improve service delivery. We asked whether they think that DHFF overall has a greater or smaller potential to improve service delivery compared to RBF (Figure 2).
Figure 2: Perceptions of which programme has the greatest potential to improve service delivery (%).
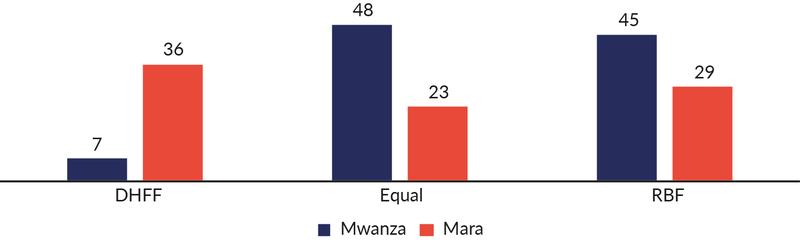
Perceptions are strikingly different across regions. While very few HWs in Mwanza (7%) believe that DHFF has a larger potential than RBF to improve service delivery, more than a third of HWs in Mara believes this to be the case. The fact that no RBF payments have yet been made in Mara is likely to contribute to this difference. On the other hand, more HWs in Mwanza than in Mara believe that RBF has a larger potential than DHFF. Yet, around 50% of HWs in Mwanza, who have quite some experience with both systems, believe that their potential to improve service delivery are equal.
When we asked more specifically about which programme so far has had the largest positive impact on the number of pregnant women who seek care, the respondents pointed more clearly at RBF in both regions (Figure 3).
Figure 3: Perceptions of which programme that so far has had the largest positive impact on the number of pregnant women who seek care (%).
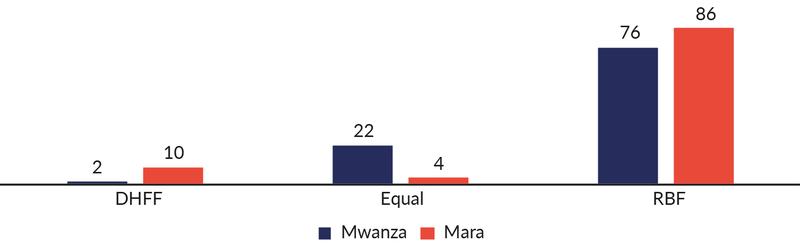
It is noteworthy that even in Mara, where RBF payments have not yet been made, the HWs think that RBF has still played an important role in increasing the number of pregnant women who seek care.
A third issue that we wanted to explore was the degree to which the two programmes had changed the mindset of HWs towards a more problem-solving attitude. We first asked to which extent RBF had changed HWs’ mindset to focus more on solving problems they face in service delivery. Almost all HWs in Mwanza (97%) answered ‘to a large extent’. Even in Mara, as many as 72% gave the same answer and only 5% said ‘to little or no extent’.
We followed up by asking whether DHFF has contributed more or less than RBF in changing health workers’ mindsets (Figure 4).
Figure 4: Perceptions of which programme that has contributed most to a more problem-solving attitude among HWs (%).
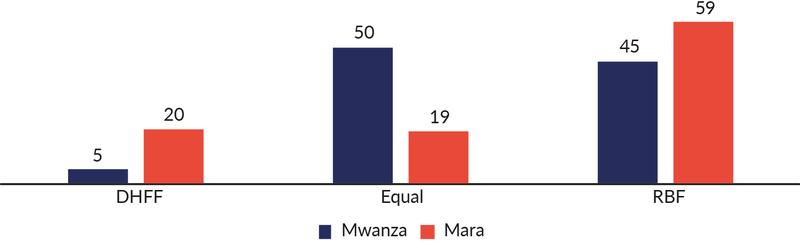
Again, we note significant differences across regions. Overall, a high share of HWs in both regions believes that RBF has a stronger impact on HWs’ mindsets than DHFF. In Mwanza, most of the other HWs believe the two programmes have equal impact, while in Mara, there is also a significant share (20%) who believes that DHFF has the largest impact on HWs’ mindsets.
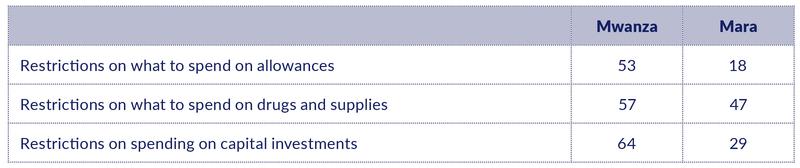
One difference between the two programmes, which might explain some of their different impacts, is that there are more stringent rules on how DHFF funds can be used compared to RBF funds. In the RBF-DHFF study, one third of the in-charges reported that restrictions on how to spend DHFF funds imposed a major constraint on their efforts to improve service delivery.
We attempted to shed more light on this issue by asking which restrictions are perceived as more or less important. The results do not point in any clear direction: between 80% and 90% of the respondents claim that all the restrictions mentioned in Table 9 are either somewhat important or very important for service delivery. Interestingly, however, HWs in Mwanza believe that the impacts of the restrictions are more severe than do HWs in Mara. One possible explanation is that they have experienced the benefits of a more liberal regime with RBF funds.
Table 9: Share of HWs who perceive restrictions on how to spend DHFF funds have a ‘very important’ negative impact on service delivery (%).
Understanding patterns in service delivery
Institutional deliveries
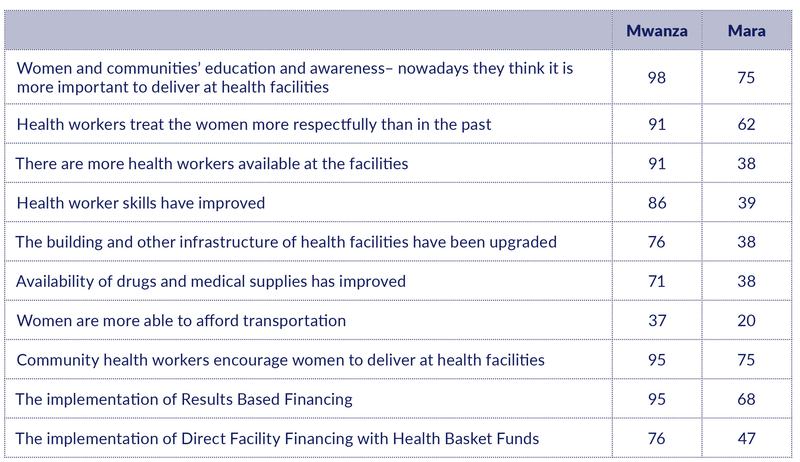
Our RBF impact study shows that a much higher share of women delivers at health facilities now compared to four years ago. We were interested in understanding what HWs perceived to be the main explanations for this change.
We first asked HWs to mention the most important reason for more institutional deliveries (open question). The responses suggest that better education and higher awareness among the pregnant women is the main reason. In Mwanza, there is also a considerable share of HWs who believe that better service quality is the main reason, while this is not the case in Mara.
We then asked HWs to rank a set of possible explanations in terms of their importance: not important, somewhat important, or very important. With few exceptions, health workers classified the options as either somewhat important or very important. Table 10 shows the share of HWs who classified the explanations as very important.
The results confirm the high importance assigned to women’s education and awareness. They also confirm that supply-side factors are more commonly believed to have played a very important role in Mwanza than in Mara.
We also notice that a considerable share of HWs in both regions think that RBF and DHFF are very important factors. However, in both regions, HWs seem to believe that RBF is an even more important factor than DHFF.
Table 10: Reasons characterised as ‘very important’ in explaining why more women deliver at health facilities (% of HWs).
The RBF impact study also showed that women who deliver at health facilities perceive that service quality has increased. To understand why, we asked HWs what they perceive as the main reason for the change. The results have not been fully analysed yet, but better education for women seems to emerge as an important factor in explaining this change as well. In other words, education empowers women to demand – and receive – health services of higher quality.
We also asked HWs to rate a set of predefined potential explanations in terms of their importance; not important, somewhat important, or very important. Very few characterised any of the explanations as not important. Table 11 shows the share of HWs who classified the various explanations as very important.
Table 11: Reasons characterised as ‘very important’ in explaining why more women experience that health workers are taking better care of them (% of HWs).

Unfortunately, we did not include better educated women among the explanations, but only asked about supply-side factors. We notice that, like above, fewer HWs in Mara than in Mwanza consider these supply-side factors to be very important. One potential explanation might be that RBF has not yet been fully implemented in Mara and has not yet affected supply-side behaviour and attitudes to the same extent as in Mwanza. Nevertheless, a high share of HWs in both regions consider RBF to have played a very important role, along with other programmes that have sensitised HWs to provide better quality care.
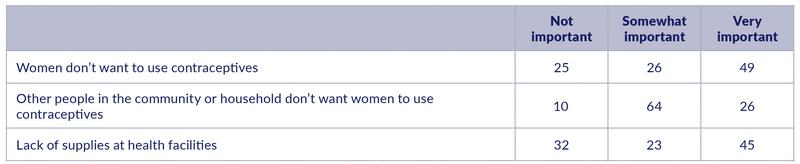
Use of contraceptives
The RBF impact study showed little or no increase in the use of modern family planning methods. In the phone survey, we followed up by asking about perceived reasons for low uptake.
Among the listed reasons, the one that was perceived as very important by the highest share of health workers (49%) was that women do not want to use contraceptives themselves, followed by lack of supplies in the health facilities (45%).
Quite a few health workers also mentioned ‘false beliefs’ as an important reason for low uptake.
Table 12: Importance of potential reasons for limited use of modern contraceptives (%).
Growth monitoring of children
Our second phone survey, conducted in 2018, demonstrated that HWs have biased beliefs about the prevalence of stunting. While the Tanzania National Nutrition Survey 2018 estimated stunting in children at 26% in Mwanza, most HWs in the region believe that the prevalence is much lower – between 0% and 10%.
We followed up in this survey by asking what health workers do as part of the routine growth monitoring of children.
Almost all HWs (99%) in both regions confirmed that they do growth monitoring of children under five years of age. Table 13 shows what HWs report to do during growth monitoring. Weight is measured by 98% in both regions. Fewer measured height (88% in Mwanza region and only 43% in Mara region).
To measure stunting, height needs to be plotted against age. This practice was reported by 72% in Mwanza and 57% in Mara (note that the options were not read out to the respondents, which may explain the apparent inconsistency between this figure and the lower share that reported to measure height).
Table 13: What do you or your colleagues do during growth monitoring? (%)
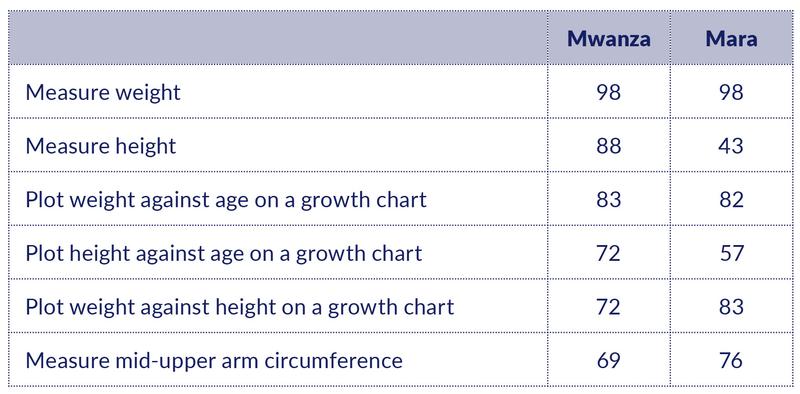
Another interesting finding is that only 42% of HWs confirmed that their facility has a length board to measure the length of children.
Overall, the practice of plotting height against age to discover stunting is less widespread than desired in both regions, and especially so in Mara. Lack of appropriate equipment to measure the height of children is likely contributing to maintaining this situation.
Results: Community health worker survey
The community health worker interviews focused on the following topics:
- RBF implementation
- RBF training and knowledge of RBF indicators
- RBF payments
- RBF and community health worker performance
- Impacts of RBF on CHW performance
- Challenges in improving RBF indicators
- Understanding patterns in service delivery
- Perceived impacts of RBF on HW behaviour
- Reasons for more institutional deliveries
- Perceptions of stunting prevalence
RBF implementation
RBF training and knowledge of RBF indicators
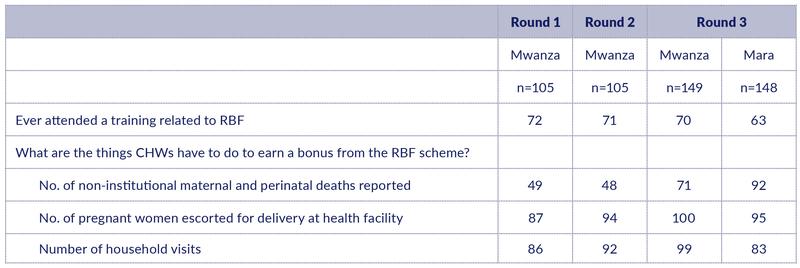
The share of CHWs who had received RBF training has remained around 70% in Mwanza in all three survey rounds. The share of trained CHWs is slightly lower in the Mara region (63%).
The knowledge among CHWs about the RBF indicators is good, also among those who have not attended RBF training. Basically, all CHWs in Mwanza and around 90% in Mara know that they earn RBF bonus by escorting women for delivery and visiting households. The knowledge about the third indicator (reporting maternal and perinatal deaths) is somewhat lower in Mwanza than in Mara, despite improvement over time.
Table 14: Training and knowledge about RBF indicators among CHWs (%)
RBF payments
There is a significant increase in the share of CHWs in Mwanza who have received any RBF payments from Round 1 (41%) to Round 3 (85%) (Table 15). RBF payments have not yet been made in Mara.
The average amounts received in the last round of payment was TSH 221,000. These payments covered 2.2 quarters on average, implying around TSH 100,000 per quarter.
Table 15: RBF payments to CHWs in Mwanza.
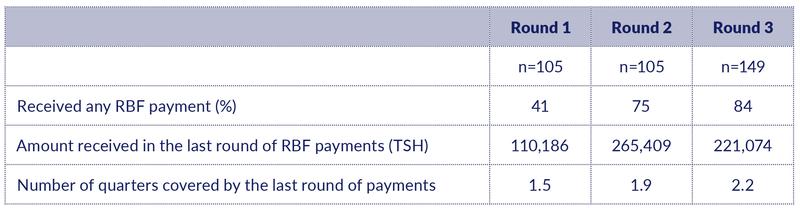
Like with the HWs, there was large variation in reported timing of the last payment: 20% had received a payment in 2020, 54% received their last payment in 2019, and 24% in 2018. Recall bias might be suspected here as well.
The delay in RBF payments was claimed by some CHWs to have reduced the number of household visits: 33% in Mwanza and 61% in Mara reported such a reduction. The difference may suggest that CHWs in Mwanza were more confident that payments would eventually arrive.
RBF and community health worker performance
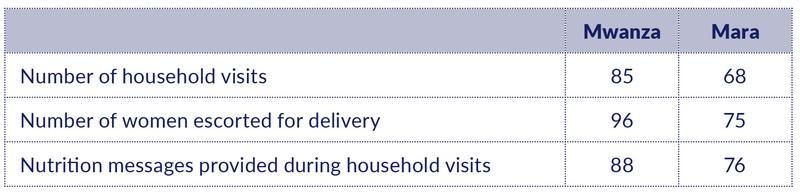
Community health worker performance
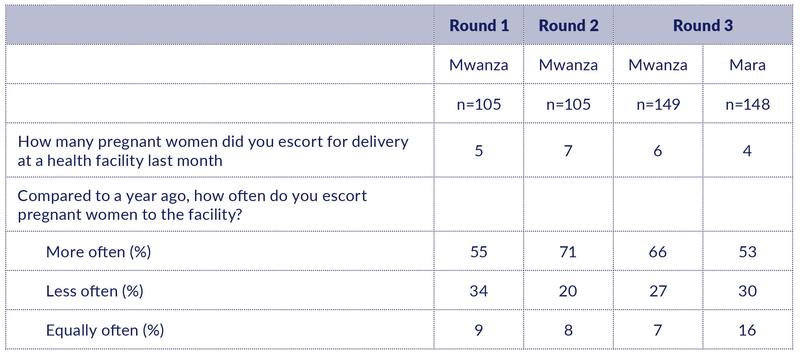
CHWs are supposed to escort women for delivery care. In previous surveys, we have asked CHWs in different ways about how many women they escort and how this number has evolved over time. In this phone survey, we asked about the number of women escorted during the last month.
The number of women escorted ranged from zero to 25, with an average of 4 in Mara and 6 in Mwanza (Table 16). CHWs in Mwanza thus escort more women for delivery than CHWs do in Mara. RBF may have contributed to this difference.
As in previous phone surveys, most CHWs perceived that they presently escort more women for delivery than they did one year ago, although there is also a significant share who reported that the number of women escorted has declined.
Table 16: Escorting women for delivery at health facilities.
We asked CHWs what they think is the most important reason why CHWs report that they now escort more women than in the past (five years ago). The almost unanimous response (96%) was that this is because of RBF.
Looking at the issue from a different angle, we asked what would happen to CHW performance if the RBF programme ends. Interestingly, as much as 86% of CHWs claim that nothing will happen to their efforts in escorting women to health facilities, and 80% believe nothing will happen to the number of household visits. The latter is not entirely consistent with the fact that a substantial share of CHWs reported that delays in RBF had caused a reduction in household visits. However, it is consistent with attitudes expressed in the RBF-DHFF study that most CHWs are used to working without pay and are therefore less affected by such changes.
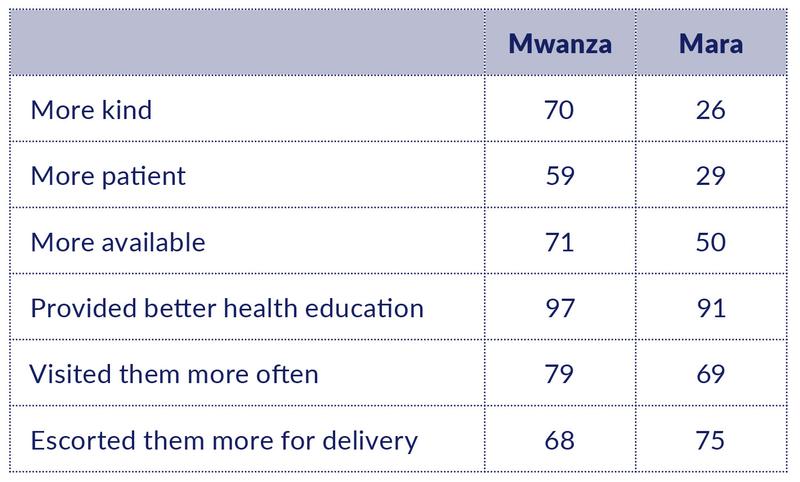
We also asked CHWs whether they believed that community members had noticed any change in CHW behaviour following the implementation of RBF, and what those changes are.
Almost all CHWs (98%) think that community members have noticed changes in CHWs behaviour, in particular an improvement in health education. Apart from the incentivised behaviours, a substantial share of CHWs, especially in Mwanza, also mention behaviours like being more kind and more available.
Table 17: What was the most important change that you think they have noticed?
The RBF programme is not implemented in isolation, but rather alongside other programmes that may also have affected CHW behaviour. The majority of CHWs named specific programmes that also have influenced their work. We then asked whether other programmes were more or less important than RBF for two of the RBF indicators as well as an additional variable that we hypothesised might be more affected by other programmes.
The results show that RBF is perceived to be of higher importance than other programmes, for all three variables, but that there is also a significant number of CHWs who rate other programmes as more important than RBF, especially in Mara.
Table 18: CHWs claiming that RBF is more important than other programmes for listed activities (%).
We were also interested in how RBF has affected the relationship between CHWs and health facilities. Improved cooperation was frequently mentioned in the RBF-DHFF study, but we did not have a quantifiable measure of the variable.
RBF was claimed to improve cooperation between CHWs and HWs to a large extent by 97% in Mwanza and 84% in Mara. Only 2% said that cooperation did not improve.
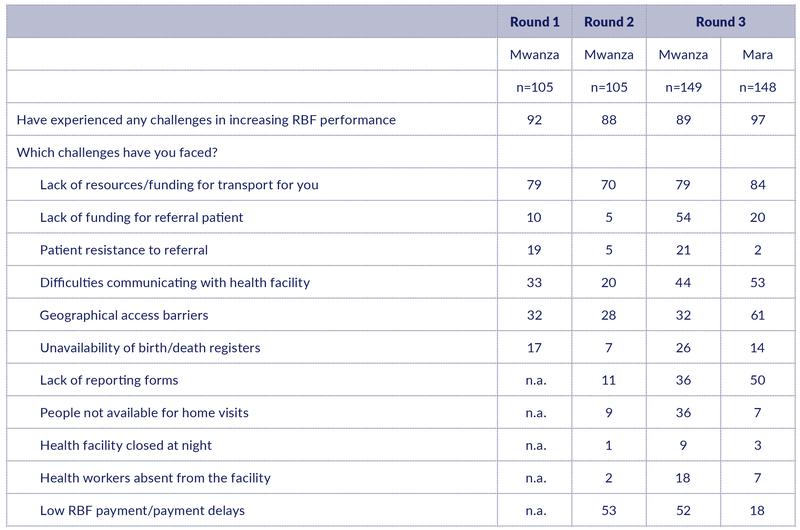
Challenges in improving performance
Most CHWs face various challenges in increasing their RBF performance (89% in Mwanza and 97% in Mara) (Table 19).
Lack of resource/funding for transport to do their work topped the list in both regions (mentioned by 79% and 84%). Other constraints mentioned by more than 50% of the CHWs are lack of funding for referring patients (Mwanza), low RBF payments or payment delays (Mwanza), geographical access barriers (Mara), difficulties communicating with health facilities (Mara), and a lack of reporting forms (Mara).
We notice that RBF payment delays are less of an issue in Mara where RBF was implemented more recently. We also notice that in Mwanza, most of the challenges are faced by more and more CHWs over time (e.g., people not being available for home visits, patient resistance, and health worker absenteeism).
Table 19: Challenges faced by CHWs in increasing RBF performance (%)
Understanding patterns in service delivery
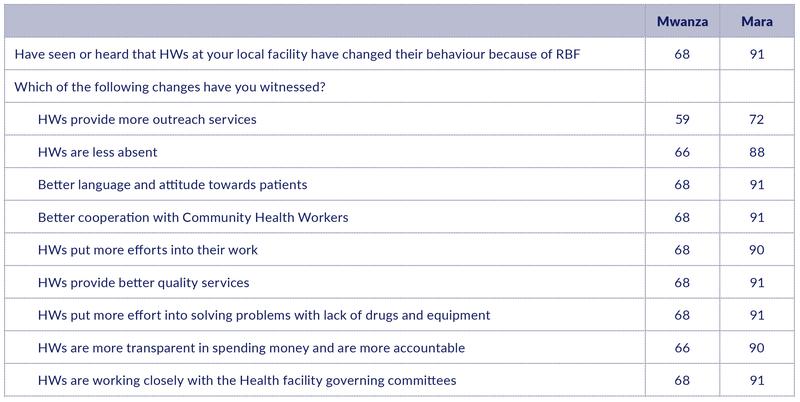
Observed changes in HW behaviour
In the RBF impact study, many HWs claimed to have changed their behaviour as a result of RBF. We wanted to triangulate this observation by asking CHWs whether they have experienced any change in HW behaviour.
In Mwanza, 68% of CHWs report that they have seen or heard that HWs at their local facility have changed their behaviour because of RBF (Table 20). In Mara, the share is much higher – 91%. We speculate that the difference might be explained by the more recent introduction of RBF in Mara, which makes it easier to make a before-after comparison.
We then listed possible behavioural changes and asked those who have experienced any change to indicate which changes they have witnessed. Since these questions were answered only by those who said that they observed any changes, the maximum scores will be 68% and 91%, respectively. Strikingly, almost all scores are very close to – or at – the maximum score (with one exception: HWs providing more outreach services). Overall, CHWs strongly support the claims made by HWs about behavioural change as a result of RBF.
Table 20: Changes in HW behaviour because of RBF, as witnessed by CHWs (%).
Institutional deliveries
We asked CHWs the same question as we did to HWs about the reasons why more women now deliver at health facilities compared to four years ago. Their responses largely confirm what HWs said.
When asked about the most important reason for the increase in institutional deliveries, CHWs in both regions point to increased education of women and communities.
We then asked CHWs to rank possible explanations in terms of their importance: not important, somewhat important, or very important. With few exceptions, CHWs classified the options as either somewhat important or very important. Table 21 displays the share of CHWs who classified the explanations as very important.
Table 21: Reasons characterized as ‘very important’ in explaining why more women deliver at health facilities (% of CHWs).
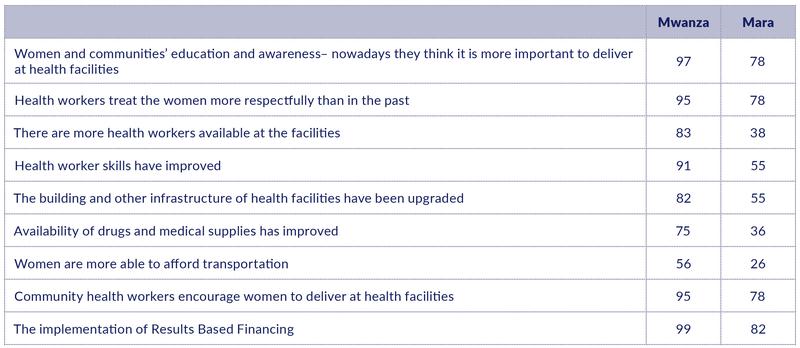
The results are strikingly similar to the results obtained by asking HWs the same question (Table 10). High importance is assigned to women’s education and awareness. Some supply-side factors are also seen by many as very important, such as women being treated more respectfully by health workers, and encouragements by CHWs. The implementation of RBF is also seen as very important by a large majority in both regions.
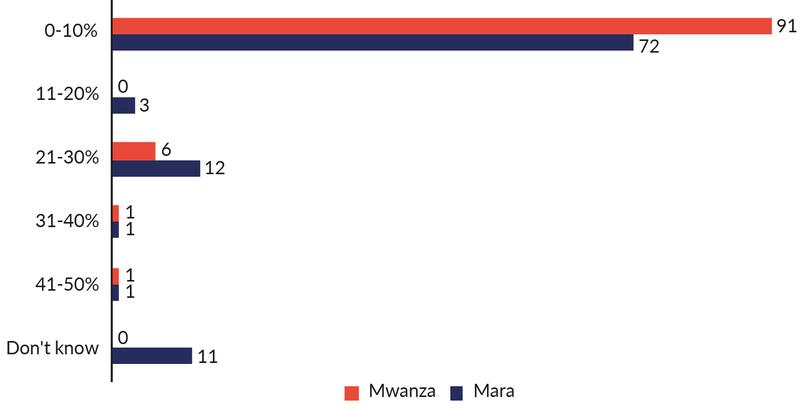
Perceptions of stunting prevalence
We asked CHWs the same questions that we asked HWs in a previous phone survey about their beliefs about stunting prevalence among children below the age of two in their district. We explained the term stunting as children being much shorter than they should be for their age because of malnutrition.
The results confirm the pattern that we observed among HWs. The beliefs are strongly biased: almost all CHWs believe that many fewer children are stunted than actually are. While the Tanzania National Nutrition Survey 2018 estimated stunting prevalence to be 26% in Mwanza and 29% in Mara, the large majority of CHWs in both regions believe that stunting prevalence is between 0% and 10%.
Figure 5: CHWs’ beliefs about stunting prevalence among children less than two years in their district (%).
Key messages
Results-based Financing (RBF)
- A declining share of health workers has received RBF training, but knowledge of RBF indicators has nevertheless improved over time.
- The share of trained community health workers is stable, and they are quite aware of the RBF indicators.
- Utilisation of OPD services and measles immunisation services are perceived by health workers as particularly difficult to increase.
- Although health workers faced very large delays in RBF payments, most claim that the delays didn’t affect the quality of services.
- Many health workers claim that quality would not be reduced if all RBF payments went to the facility rather than partially to staff bonuses.
- Community health workers also faced payment delays, and some say they didn’t do as many household visits as a consequence.
- Lack of funds for transport continues to be the main challenge for community health workers in improving their RBF performance.
- Community health workers confirm that RBF has positively affected the behaviour of health workers.
Direct Health Facility Financing (DHFF)
- The majority of health workers didn’t receive DHFF training.
- Training could have been improved by taking more time to explain things better. Limited computer skill among participants should also be taken into account.
- Many health workers perceive that restrictions on how to use DHFF funds have a very important negative impact on service delivery.
- The new digital tool for planning and budgeting (PlanRep) is not sufficiently in use. Reasons include low competence, limited user-friendliness, and technical issues.
- Access to stable electricity, computers, and internet is still too low.
Understanding patterns in service delivery
- Increase in institutional deliveries is primarily attributed to women’s and communities’ education and awareness, as well as to attitudinal changes among health workers and community health workers.
- RBF is perceived to have had a larger impact than DHFF on institutional deliveries.
- Community health workers report that they escort more women for delivery than in the past and that the main reason for the change is RBF. At the same time, they claim that ending the RBF would not reduce their efforts in this regard.
- The limited increase in the use of modern family planning methods is attributed as much to low demand as to limited supplies.
- While most facilities plot the children’s weight against age, many fewer plot the height against age, presumably because of a lack of length boards. This may explain why health workers severely underestimate the prevalence of stunting.
- Community health workers also severely underestimate the prevalence of stunting.
Ottar Mæstad





![Corona überleben: Die Figur der:s Überlebende:n als Trägerin von Hoffnung und Angst in den Politiken einer Krise im Werden [Surviving Corona: The figure of the survivor as bearer of hope and fear in the politics of an emerging crisis]](http://www.cmi.no/img/400/18259-Corona-und-mediale-ffentlichkeiten.png)


