Towards harmonised financing of frontline health service providers in Tanzania
How to cite this publication:
Ottar Mæstad, Peter Binyaruka (2021). Towards harmonised financing of frontline health service providers in Tanzania. Bergen: Chr. Michelsen Institute (CMI Brief 2021:5)
This brief discusses what we can learn from recent experiences with direct health facility financing in Tanzania for the future design of a more harmonised system for financing of frontline service providers.
CMI Report 2021:07: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #1
CMI Report 2021:08: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #2.
CMI Report 2021:09: Direct health facility financing in Tanzania. Process evaluation. Phone Survey #3
CMI Report 2021:10: Direct Financing of Health Facilities. Experiences from financing reforms in Tanzania.
Key messages
• Direct financing of frontline service providers seems to increase efficiency and may also increase transparency and accountability.
• Better training is needed for health providers on how direct financing mechanisms work.
• Frequent monitoring is important for sustaining a focus on outputs and performance at health facilities.
• More flexibility in budgeting and spending can further improve service delivery.
• Health worker bonuses may not be a necessary part of direct financing systems.
• Output-based financing needs to be combined with other mechanisms to ensure both efficiency and equity.
• A problem-solving attitude needs to be cultivated along with the implementation of direct financing of frontline service providers.
Introduction
The Tanzanian government is committed to ensuring universal health coverage by providing quality health services to all citizens without risk of financial hardship.
Financial resources for health are scarce and need to be carefully managed to ensure efficient and equitable service provision. Total health expenditures per capita were 28.5 USD in 2017, or 2.5% of GDP. This is well below commonly used benchmarks for achieving universal health coverage (86 USD per capita or 5% of GDP).
Tanzania is in a process of reforming its health financing system to achieve universal health coverage. There has been a partial transition from input-based to output-based financing, and some funds are now flowing directly from the Ministry of Finance and Planning to health facilities, which enhances autonomy in prioritization of spending at the facility level. This process started with the implementation of Results-based Financing (RBF) in nine regions and continued with the nationwide implementation of Direct Health Facility Financing (DHFF) of Health Basket Funds – the pooled donor funding of the health sector. The government has also made steps to harmonise the financing system, for instance through the implementation of digital budgeting, planning and accounting tools at the facility level.
The financing system nevertheless remains fragmented, with different guidelines for budgeting, spending, and reporting for government funds, Health Basket Funds, Results-based Financing, user fees and various insurance mechanisms. Moreover, a large share of donor funding is off-budget and managed through vertical programmes focusing on single diseases / health issues. This creates inefficiencies, partly because of the complexities of the system, and also because it is not straightforward to substitute between funding sources. The latter challenge is compounded by unreliable funding streams due to lack of timely release of budgeted resources.
A more harmonised health facility financing system is needed, but what should such a system look like? What is the optimal design to promote efficiency, equity, quality, and accountability? This brief sheds light on these questions by drawing on recent research on the experiences with Results-based Financing and Direct Health Facility Financing of the Health Basket Fund.
Key features of the current financing system
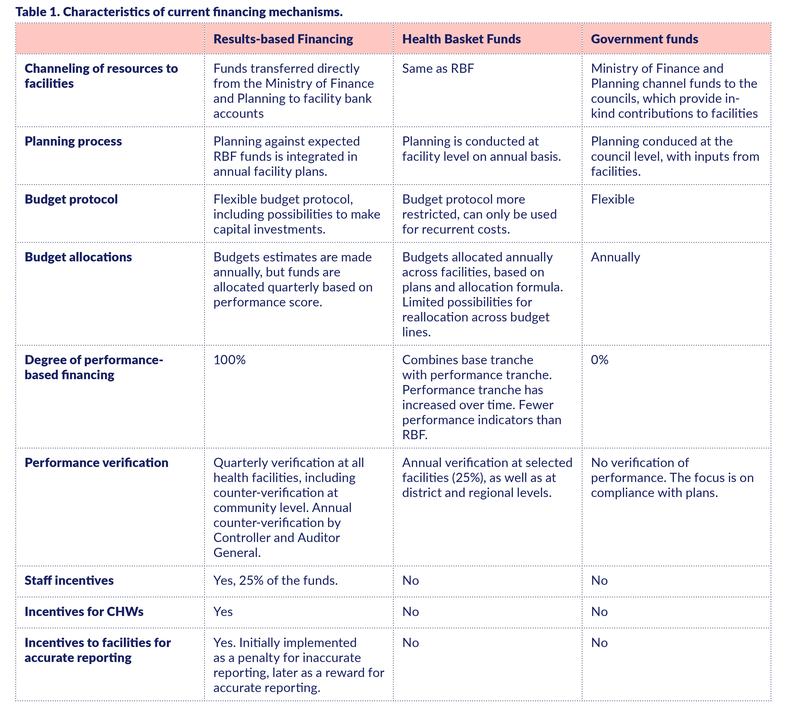
As background, this section compares key features of three major funding mechanisms for health facilities in Tanzania: (i) government funds allocated through councils, (ii) direct allocation of Health Basket Funds, and (iii) direct allocation of Results-based Financing.
Both government funds and Health Basket Funds have traditionally been provided as in-kind contributions; funds were transferred to councils, which provided facilities with service delivery inputs based on annual plans. Equity considerations across and within councils were taken into account through the allocation formulas.
In contrast, the Results-based Financing (RBF) mechanism, implemented in nine regions from 2016 onwards, allocates funds quarterly directly from the Ministry of Financing and Planning to health facility bank accounts, based on reported outputs and adjusted for a quality score. 25% of the funds are allocated as bonuses to facility staff, with the remaining amount going to the health facility, with considerable autonomy in budgeting and spending. Bonuses are also provided to community health workers based on performance outcomes. To enhance accountability, quarterly verification visits are implemented at all health facilities prior to RBF payments, and incentives are provided for accurate reporting.
From 2018, some key features of RBF were adopted in the new mechanism for transferring Health Basket Funds directly to facility bank accounts rather than to the councils. With these direct transfers, facilities also had increased autonomy in planning and budgeting, and over time the scheme also incorporated selected output and quality indicators in the allocation formula. However, the budget protocol is more restrictive than with RBF (e.g., Health Basket Funds cannot be used for capital investments, and there are restrictions on how much can be spent on various items), it has many fewer output and quality indicators than RBF, it mandates many fewer verification visits (only 25% of the facilities annually), and Health Basket Funds do not include bonuses for health workers. The main differences between the three financing mechanisms are summarized in Table 1.
Drawing the best from different mechanisms
Below are some of the lessons drawn from our recent research on Results-based Financing and direct financing of Health Basket Funds in the Mwanza and Mara regions. Both regions have received direct financing of Health Basket Funds since 2018, while RBF was implemented in Mwanza in 2016 and in Mara in late 2019 (but no RBF payments had yet been made in Mara at the time of this research).
Direct financing of frontline providers seems to increase efficiency. We find that RBF improved the availability of drugs, improved overall service quality, and increased the provision of some, but not all, services. Figures 1 and 2 illustrate the development in drug availability and service quality in delivery care in Mwanza and Mara between 2016 and 2020.
Figure 1: Drugs in stock (average across 34 drug items), %.
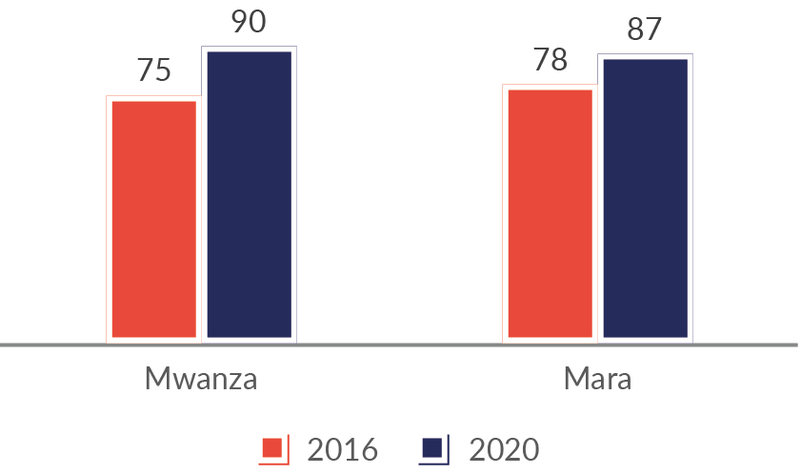
Source: Health facility survey. N=150.
Figure 2: Quality of delivery care (average score across 32 indicators), %.
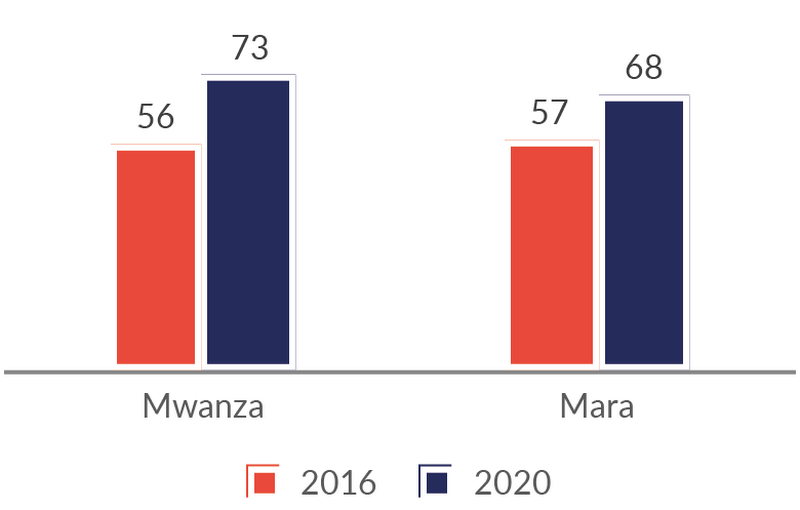
Source: Health facility survey. N=150.
The fact that improvements have consistently been stronger in Mwanza than in Mara suggests that RBF increased efficiency. RBF made health workers improve the content of care, and they dealt with patients in a more responsive manner. Facility managers claimed that output-based financing was an important driver for these changes.
Health workers and managers held the view that direct financing of the Health Basket Fund also improved efficiency. For example, health managers claim that this mechanism reduced loss of time and resources compared to previous bureaucratic processes to access funds from councils. Enhanced provider autonomy also contributed as it increased local ownership in the development and implementation of plans, similar to what happened with RBF.
Direct financing of providers may also increase transparency and accountability. Direct financing of the Health Basket Fund increased transparency with respect to the allocation of resources across facilities. Both mechanisms strengthened local governance and accountability mechanisms by empowering Health Facility and Governance Committees (HFGCs) to take a more active role in overseeing facilities, planning, and budgeting. The number of meetings per year in HFGCs increased by 68% in Mwanza and 32% in Mara from 2016 to 2020. However, direct financing also creates new challenges, including stronger incentives for misreporting. Opportunities for misreporting are probably more limited with RBF than with direct financing of the Health Basket Fund, due to more frequent verification visits.
Better training is needed for health providers on how direct financing mechanisms work. Solid understanding of the funding mechanisms is crucial for inducing deswired behavioural changes. It is particularly important that providers understand how to obtain more funds. Health workers were able to mention around 50% of the performance indicators for RBF and Health Basket Funds on average. A substantial share of facility in-charges do not know very well how to obtain direct financing (Figure 3) and report that training has not been adequate, especially on direct financing of Health Basket Funds (Figure 4). This suggests that training can be improved, in particular on the Health Basket Fund mechanism.
Figure 3: The extent to which facility in-charges in Mwanza/Mara know how to obtain RBF and Health Basket Funds (%).

Source: Health facility survey. N=150.
Figure 4: The extent to which facility in-charges have received adequate training in RBF and direct financing with Health Basket Funds (%).

Source: Health facility survey. N=150.
Our data also suggests that quite a small percentage of health workers have been trained in direct financing of Health Basket Funds as compared to that of RBF. However, those who were trained also revealed a limited satisfaction with the training due to limited computer skills among participants and a lot of material being covered in a short time. They also mentioned that the material was complicated and that trainers did not explain things in detail. These are areas that require attention in future training activities.
Our research also indicates the use of the new planning and budgeting tool (PlanRep) can be enhanced through training that ensures facility managers can use the tool properly and understands how it can be helpful to them. Technical challenges with computers and electricity supply also contribute to less-than-optimal use of the tool.
Frequent monitoring is important for sustaining the focus on outputs and performance. Health facility in-charges claim that quarterly verification visits with RBF have contributed importantly to improved service delivery, because it has ensured a continuous focus on performance. This is an interesting finding, since one might think that the existence of bonus payments and quarterly reporting would be sufficient to main such a focus. One possible explanation might be that visits by external verifiers help keep health workers’ attention on the importance of improving performance.
With direct financing of Health Basket Funds, verification visits occur much less frequently than with RBF, only once every fourth year on average. Combined with fewer incentives for health workers, there are thus fewer mechanisms that maintain and reinforce the focus on performance. More frequent verification visits or other mechanisms for ensuring a continuous focus on performance should therefore be considered.
Flexibility in budgeting and spending is important for improved service delivery. One third of the in-charges reported that restrictions on how to spend Health Basket Funds imposed a major constraint on their efforts to improve service delivery. In Mwanza, where health workers have extensive experience with both the Health Basket Fund mechanism and the more flexible RBF spending protocol, more than 50% of the health workers claimed that restrictions on spending on capital investments, drugs and supplies, as well as allowances related to Health Basket Funds, all have a very important negative impact on service delivery.
At the same time, there may be good reasons not to fully decentralize these decisions. For instance, there is a need for holistic planning of the health infrastructure in a council, and all infrastructure decisions should therefore not be delegated to the facility level. We nevertheless recommend looking into how the various funding mechanisms work together to ensure a sound balance between decentralized decision-making and top-down regulation on budgeting and spending.
Health worker bonuses may not be required for strengthening health worker performance. Our findings point in different directions when it comes to the importance of personal bonuses in explaining positive effects of RBF on service delivery. On the one hand, facility in-charges claim that incentives (both for facilities and health workers) were among the most important aspects of RBF in explaining improved service provision. On the other hand, there is no evidence that performance declined significantly during long periods of delays in RBF payments. Service output was maintained, and most health workers claim that quality and motivation also was maintained. While this can be explained by health workers continuing to believe that they sooner or later would be paid, it can also indicate that these incentives are not crucial. We therefore followed up by asking health workers what would happen to quality if all performance payments were allocated to health facilities, and nothing went to health workers. Although health workers have incentives to overstate the negative implications of such a shift, 58% of health workers said that this would not have any negative impact on service quality.
Figure 5: Perceived effect of letting all RBF payments go to the health facility (%).
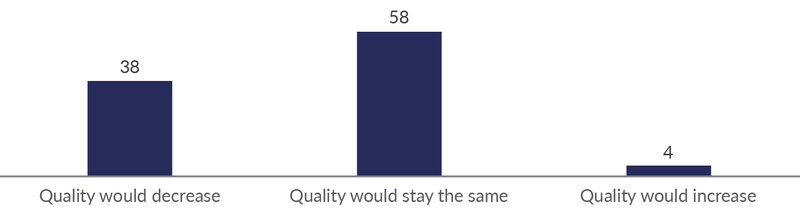
Source: Phone survey. N=293.
Some health workers are likely to reduce performance if there were not any incentives for staff. But such incentives could be given in more indirect ways than through bonuses. The opportunity to spend up to 15% of Health Basket Funds on allowances can, for instance, be an indirect way of providing incentives for staff, as allowances can be quite generous.
Output-based financing needs to be combined with other mechanisms to ensure both efficiency and equity. An important question in the design of a direct facility financing system is to which extent the system should rely on output-based financing. Should all funding be based on output (and quality) indicators, as in RBF, or should some funds be allocated based on other indicators, as in the allocation of Health Basket Funds?
Health facilities differ in their cost structure. Remote facilities have higher transport costs, and they may also need extra resources to be able to attract qualified health personnel. For equity reasons, it is therefore reasonable that remote facilities receive additional resources. Allocation of extra resources based on remoteness from district headquarters, as is presently part of the Health Basket Fund allocation formula, is therefore reasonable from an equity perspective.
Health Basket Funds are presently also allocated with more resources going to facilities with a high catchment population. This is a reasonable approach when there is limited output-based financing, with few output indicators covering a small portion of the services. The opposite is the case when there are output indicators for most services. Equity considerations may then imply that those facilities with a low catchment population should be compensated, because these facilities typically have higher fixed costs per patient (e.g., infrastructure costs).
A problem-solving attitude needs to be cultivated along with the implementation of direct financing. One of the ideas behind direct financing of frontline providers is that it will encourage health workers to address obstacles in provision of quality services. The behavioural response does however not only depend on the technical design of the financing system, but also on how the system is perceived by the health workers. Our interviews with health workers suggest that RBF has generated a stronger problem-solving attitude among health workers than has the Health Basket Fund mechanism, for instance, in how they approached the budgeting process. In a follow-up phone survey, 52% of the respondents confirmed this impression.
Figure 6: Perceptions of which programme that has contributed most to a more problem-solving attitude among HWs (%).
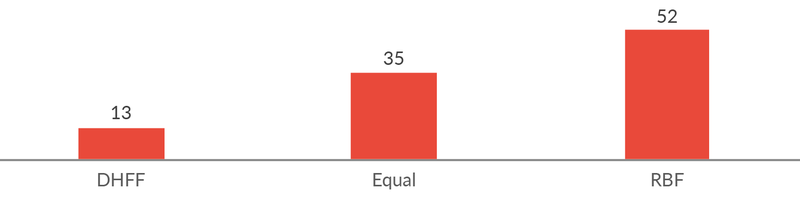
Source: Phone survey. N=290.
One possible explanation is that direct financing of Health Basket Funds is perceived by many primarily as a mechanism to avoid bureaucratic processes of obtaining funds and not so much as an opportunity to expand the resources of the facility. This is consistent with our finding that knowledge of how to obtain more resources from Health Basket Funds is not as strong as in the case of RBF. Such aspects were perhaps not a key element of training about Health Basket Funds, as output-based financing was not part of the mechanism from the beginning but was phased in gradually over time. Perhaps it is also the case that the scheme itself in other ways does not cultivate a problem-solving attitude to the same extent as does RBF. Whatever the reason, there seems to be something to learn from the way RBF has come to be perceived by health workers that can and should inform the further development of direct financing of frontline service providers in Tanzania.

Ottar Mæstad




![Corona überleben: Die Figur der:s Überlebende:n als Trägerin von Hoffnung und Angst in den Politiken einer Krise im Werden [Surviving Corona: The figure of the survivor as bearer of hope and fear in the politics of an emerging crisis]](http://www.cmi.no/img/400/18259-Corona-und-mediale-ffentlichkeiten.png)


